Unaddressed Denials, Growing AR
Failure to address denied claims promptly can lead to significant revenue losses and cash flow issues for healthcare providers
Failure to address denied claims promptly can lead to significant revenue losses and cash flow issues for healthcare providers
Underpaid claims often go unnoticed, resulting in reduced reimbursement and financial strain on healthcare practices
Partially paid claims that are not followed up can accumulate, causing substantial revenue shortfalls over time
Claims that receive no response from payors can be overlooked, leading to potential losses if not diligently tracked and managed
Without a robust system to monitor and manage claims, providers struggle to keep track of denials, underpayments, and unpaid claims
Inadequate knowledge of denial resolution processes can hinder effective claim recovery and result in prolonged payment delays
Providing care to ineligible patients can lead to non-reimbursable claims, increasing financial burdens on healthcare facilities
Failing to collect patient co-pays, deductibles, and other responsibilities can significantly impact the revenue cycle
A lack of transparency and control over the billing process can create confusion and inefficiencies, undermining financial performance
High turnover and excessive workload among billing staff can lead to errors, delays, and a decrease in overall productivity
Frequent changes in payor adjudication policies require constant updates to billing practices, adding complexity and administrative burden
Inefficient billing processes and missed revenue opportunities can prevent healthcare providers from achieving their full financial potential
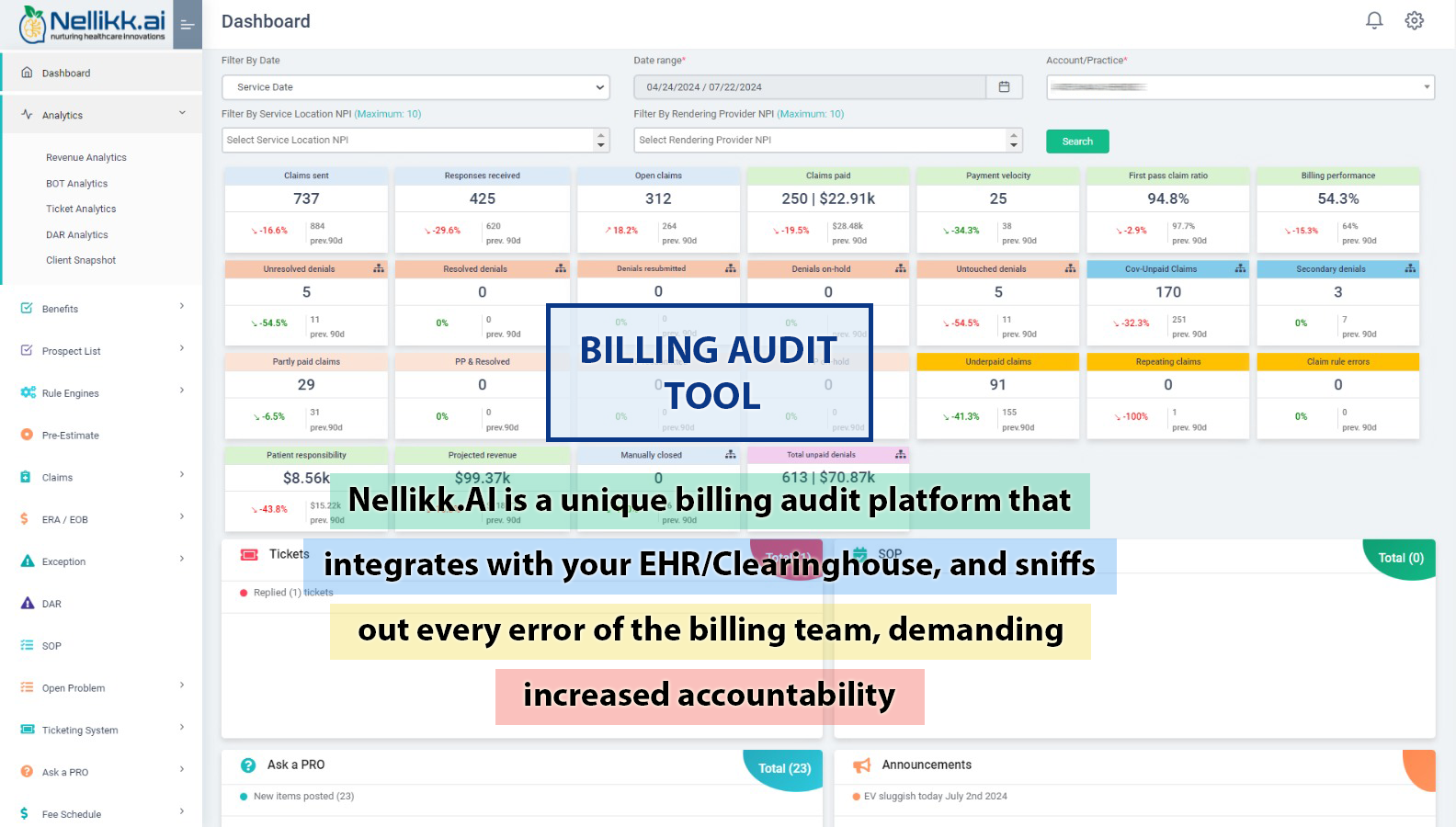
Stay on top of critical revenue metrics, raise and assign questions and tickets.
Revenue focused perspective enlarges opportunities. Makes staff accountable for missed opportunities.


Customized benefits reports tailored to each practice specialty provide precise and relevant information, streamlining the verification process. Perform manual or automated eligibility and benefits verification on a single or bulk basis
Drastically reduce claim status verification calls by 70% with this feature. Search, and filter through hundreds of open claims, and submit tasks with a click, transforming hours of work into minutes
Categorize and resolve denials with recommendations received from top analysts and benefit from Al-powered resolution suggestions for every denial
Optimize your pricing strategy with our ML-based fee schedule analyzer, ensuring competitive and compliant fee structures
This feature, mines visit history for potential routine and follow-up appointments, to ensure patient care, and busy schedule of providers
Monitor and improve your financial performance with our KPI tracker, designed to boost revenue and operational efficiency
Gain insights into productivity and compensation with WRVU-based analytics, aligning efforts with financial goals
Plan confidently with accurate revenue projections, maintaining less than 5% tolerance for financial stability
Provide accurate cost estimates to patients with pre-estimates driven by our ML-based fee schedule, enhancing transparency and satisfaction